ARRS Roles in Primary Care
Embedding the ARRS roles
Nottinghamshire Alliance Training Hub (NATH) is supporting the Primary Care Networks (PCNs) to understand how the new roles will be embeded across Nottingham & Nottinghamshire Integrated Care System (ICS). As the local Training Hub, we will support future workforce planning as one of our six core functions.
Index of the ARRS roles
In total there are 16 new roles. Information about them is developing all the time. These are:

Advanced Practitioner
Advanced Practitioners are an integral part of the 21st century NHS workforce as new models of care are transforming the way patients are treated. Advanced Practitioners work at level 7 across the four pillars of advanced practice – clinical, management/leadership, research and education.
They offer multiple benefits to the health service and the population. They bring more holistic care to patients, support continuity of care and extend the scope of practice across traditional boundaries. This leads to a greater focus on prevention, more personalised care, a more efficient team, a faster response to patient needs and better outcomes.
They are instrumental in supervising the multi-professional team in primary care. They attract and lead research and audits, as well as manage highly complex, high-risk patients. They have a leadership role in the ICS around pathways and population health.

Care Coordinator
Care Coordinators play an important role within a PCN to proactively identify and work with people, (including the frail/elderly and those with long-term conditions), to provide coordination and navigation of care/support across health and care services.
Care Coordinators could potentially provide extra time, capacity, and expertise to support patients in preparing for or in following-up clinical conversations they have with primary care professionals. They will work closely with the GPs and other primary care professionals within the PCN to identify and manage a caseload of identified patients. This makes sure that appropriate support is made available to them and their carers, and ensures that their changing needs are addressed. This is achieved by:
Bringing together all the information about a person’s identified care and support needs
Exploring options to meet these within a single personalised care and support plan, based on what matters to the person

Clinical Pharmacist
Clinical Pharmacists work in primary care as part of a multidisciplinary team in a patient facing role. They clinically assess and treat patients using expert knowledge of medicines for specific disease areas. They will be prescribers, or if not, can complete an independent prescribing qualification following completion of the 18-month Centre for Pharmacy Postgraduate Education (CPPE) pathway.
They work with and alongside the general practice team, taking responsibility for patients with chronic diseases and undertaking clinical medication reviews to proactively manage people with complex polypharmacy, especially for the elderly, people in care homes and those with multiple comorbidities.
Clinical Supervision Bulletins
Nottinghamshire Alliance Training Hub (NATH) have developed various Clinical Supervision Bulletins to share best practice. This includes:
A Brief Guide to Effective Support of Pharmacists in GP Practice
Handling Concerns about Clinical Pharmacists
Developing Structured Medication Reviews
Developing Pharmacists Post Centre for Pharmacy Postgraduate Education (CPPE) Pathway
Introduction to Workplace-Based Assessments

Dietitian
Dietitians are healthcare professionals that diagnose and treat diet and nutritional problems, both at an individual patient, and wider public health level. They work in a variety of settings with patients of all ages. Dietitians support changes to food intake to address diabetes, food allergies, coeliac disease and metabolic diseases. They also translate public health and scientific research on food, health and disease into practical guidance to enable people to make appropriate lifestyle and food choices.

Digital and Transformation Lead
The Digital and Transformation Lead role was introduced as a reimbursable role via the ARRS in October 2022. The key objective of the role is to support PCNs and their practices to deliver ongoing improvement to services utilising data to improve quality, efficiency, to support population health management, workforce or estate planning.
New guidance on this role, alongside an example Job Description and an FAQ section have now been published on FutureNHS (log in required) in order to support PCNs in implementing this role.

First Contact Physiotherapist
First Contact Physiotherapists (FCPs) are qualified autonomous clinical practitioners who can assess, diagnose, treat and manage musculoskeletal (MSK) problems and undifferentiated conditions. Where appropriate, they can discharge a person without a medical referral. FCPs can be accessed directly by self-referral or by staff in GP practices who can direct patients to them. This enables a rapid and accurate diagnosis and management plan to streamline pathways of care.

General Practice Assistant
As part of the wider team in general practice, General Practice (GP) Assistants provide a support role, carrying out administrative tasks combined, in some areas, with basic clinical duties. They focus on supporting General Practitioners in their day-to-day management of patients, specifically aimed at reducing the administrative burden, making the best use of consultation time and supporting those particularly vulnerable to isolation who are regular attenders at the practice.
Development of the role depends on a range of factors – patient needs, existing skills mix, culture, and having the staff, time and financial resource to invest in work-based learning, mentorship and supervision.

Health and Wellbeing Coach
Health and Wellbeing Coaches (HWBCs) will predominately use health coaching skills to support people with lower levels of patient activation. This helps to develop the knowledge, skills, and confidence to become active participants in their care so that they can reach their self-identified health and wellbeing goals. They may also provide access to self-management education, peer support and social prescribing.
HWBCs will use a non-judgemental approach that supports the person to self-identify existing issues and encourages proactive prevention of new and existing illnesses. This approach is based on using strong communication and negotiation skills, supports personal choice and positive risk-taking, addresses potential consequences, and ensures people understand the accountability of their own decisions based on what matters to the person.
They will work alongside people to coach and motivate them through multiple sessions, supporting them to self-identify their needs, set goals, and help them to implement their personalised health and care plan.

Mental Health Practitioner
Mental health practitioners support adults whose needs cannot be met by local talking therapies, but who may not need ongoing care from secondary mental health services. The practitioner can be taken on by a wide range of clinical and non-clinical roles with mental health expertise (ranging from Band 4-8a), such as a community psychiatric nurse, clinical psychologist, mental health occupational therapist or a peer support worker.
Mental health practitioners for children and young people can be developed to meet a wide range of needs, from early identification and intervention in primary care, to more targeted or intensive support and interventions as part of a joined-up approach with children and young people’s community mental health services. The exact scope of the role and job description should be agreed between the PCN and the NHS trust but could include children wellbeing practitioners, community mental health nurse, and cognitive behavioural and family therapists.
As this is part of the wider transformation and expansion of community mental health services, the practitioner will be employed by the secondary mental health provider and will operate as a fully embedded member of the PCN multidisciplinary team. They will act as bridge between primary care and secondary mental health services and can facilitate onward referral to a range of services to meet patients’ needs.

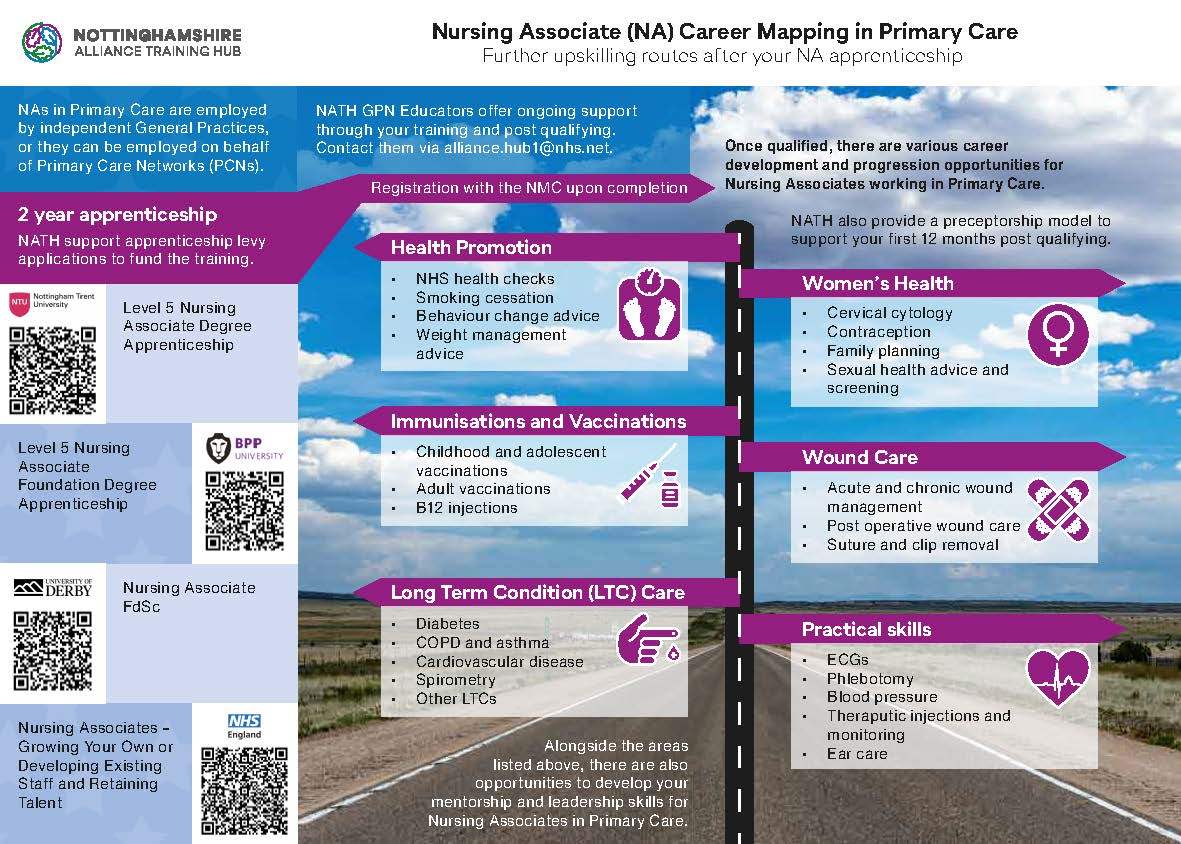
Nursing Associate and Trainee Nursing Associate
The Nursing Associate is a new support role in England that bridges the gap between healthcare support workers and registered nurses to deliver hands-on, person-centred care as part of the nursing team. Nursing Associates work with people of all ages in a variety of settings in health and social care.
The role was introduced in response to the Shape of Caring Review (2015), to help build the capacity of the nursing workforce and the delivery of high-quality care. It will be a vital part of the wider health and care team and aims to:
Support the career progression of healthcare assistants
Enable nurses to focus on more complex clinical work
Increase the supply of nurses by providing a progression route into graduate-level nursing
Case Study – Trainee Nursing Associate
What do your daily tasks look like?
Review appointments including observations and phlebotomy
ECGs (Electrocardiograms)
Wound care
Urinalysis
Immunisations
NHS Health Check appointments and follow up
Health promotion
Escalating care
Providing support for our registered carers
What’s the biggest difference you have made in this role?
Being able to provide more comprehensive support to the patients I care for. Whether that be through escalating concerns to a GP, or signposting to services to address the wider determinants of health.
What do you enjoy about your role?
I enjoy gaining valuable experience during my placements within the four fields of nursing (mental health, learning disabilities, adult and paediatrics). I like the fact that I can care for patients in a more holistic manner and being able to learn and work at the same time!
What challenges have you found working in this role?
The transition from Healthcare Assistant to Trainee Nursing Associate has been difficult for the team to adapt to as I have been in my previous role for several years. Being the first Nursing Associate, I have had to fly the flag for my role and break down barriers. However I have enjoyed helping people to understand where my role fits into a general practice setting.

Your Future Nurses
Following the introduction of the nursing degree apprenticeship, the nursing associate role, and initiatives such as the return to practice, there are now more options than ever to develop registered nurses within the workforce, as well as the traditional university route.
Starting from January 2021, a blended nursing degree combining digital and traditional elements of learning will be available to attract those who may previously have had barriers to a nursing career. Learn more about the different routes to recruiting your nursing workforce and ways to increase your nursing supply by visiting the NHS Employers website.

Occupational Therapist
Occupational Therapists (OTs) support people of all ages with problems resulting from physical, mental, social, or development difficulties. OTs provide interventions that help people find ways to continue with everyday activities that are important to them. This could involve learning new ways to do things or making changes to their environment to make things easier.
As patients’ needs are so varied, OTs help GPs to support patients who are frail, with complex needs, live with chronic physical or mental health conditions, manage anxiety or depression, require advice to return or remain in work, and need rehabilitation so they can continue with previous occupations (activities of daily living).

Paramedic
A paramedic in primary care can provide a rapid response to deteriorating patients and patients with long-term conditions, minor injuries, and minor illness. They can also support patients who require wound care, have fallen, have musculoskeletal problems, and have urinary tract or respiratory infections. Paramedics can supply a range of medicines through patient group directions, including antibiotics and analgesics.
Paramedics can support PCNs in responding to on the day demand by offering telephone triage or undertaking home visiting. They can also support PCNs to improve access to care by managing minor ailments and seeing patients in care homes.
Resource:

Pharmacy Technician
Pharmacy Technicians play an important role within General Practice and complement the work of Clinical Pharmacists through utilisation of their technical skillset. Their deployment within primary care settings allows the application of their acquired pharmaceutical knowledge in tasks such as audits, discharge management, prescription issuing, and where appropriate, informing patients and other members of the Primary Care Network (PCN) workforce. Work is often under the direction of Clinical Pharmacists, and this benefit is realised through the creation of a PCN pharmacy team.

Physician Associate
Physician Associates (PAs) are healthcare professionals with a generalist medical education who work alongside doctors providing medical care as an integral part of the multidisciplinary team. Physician Associates are dependent practitioners who work under the supervision of a fully trained and experienced doctor. They bring new talent and add to the skill mix within teams, providing a stable, generalist section of the workforce which can help ease the workforce pressures that the NHS currently faces.

Podiatrist
Podiatrists are healthcare professionals who have been trained to diagnose and treat foot and lower limb conditions. Podiatrists provide assessment, evaluation and foot care for a wide range of patients, which range from low risk to long-term acute conditions. Many patients fall into high risk categories such as those with diabetes, rheumatism, cerebral palsy, peripheral arterial disease and peripheral nerve damage.

Social Prescribing Link Worker
Health outcomes are intrinsically linked to social circumstances. Social factors often influence whether a person develops a health problem, and conversely, living with a health problem may adversely impact a person’s social situation. Social prescribing aims to address some of the wide range issues that contribute to or result from the presence of a health problem, and help a person connect with their community.
Social prescribing enables all primary care staff and local agencies to refer people to a link worker. Social Prescribing Link Workers (SPLWs) give people time and focus on what matters to the person as identified through shared decision making or personalised care and support planning. They connect people to community groups and agencies for practical and emotional support.
They work within multidisciplinary teams and collaborate with local partners to support community groups to be accessible and sustainable, and help people to start new groups. Social prescribing complements other approaches such as ‘active signposting’.
Link workers typically support people on average over 6-12 contacts (including phone calls, meetings and home visits) with a typical caseload of 200-250 people per year, depending on the complexity of people’s needs and the maturity of the social prescribing scheme.


